This edition of Africa in Fact was planned early this year with no inkling that two months later the world would be engulfed by a health crisis that has not only revealed weaknesses in healthcare systems in countries both rich and poor, but has demonstrated that the difference between good and bad governance can quite literally be a matter of life or death.
This edition of Africa in Fact was planned early this year with no inkling that two months later the world would be engulfed by a health crisis that has not only revealed weaknesses in healthcare systems in countries both rich and poor, but has demonstrated that the difference between good and bad governance can quite literally be a matter of life or death.
COVID-19 caught the world by surprise, although scientists had repeatedly warned that a pandemic of this nature was possible, even likely. Nevertheless, the scale of the health, economic, and social consequences would have been unimaginable to most of us a year ago.
Inevitably, the articles originally planned for this edition have been overshadowed by the COVID-19 crisis, which has been brutal in laying bare Africa’s fragile health systems and exposing years of under-expenditure on public healthcare. Having said that, the continent as a whole has defied the predictions of international experts who feared Africa would be worst hit by the pandemic because of its high disease burden and fragile health systems.
By mid-August, Africa had just over a million COVID-19 cases and about 26,000 recorded deaths, compared to countries like the United States and Brazil where denial and bad leadership is clearly to blame for a mortality rate of more than 300,000 people between them by 24 September.
Health experts have cited Africa’s youthful population as one reason for the relatively low numbers recorded – and the lack of reliable data across regions might well be a factor, too – but as Paul Adepoju reports from Nigeria, and Andrew Panton writes about the Ebola outbreaks in West Africa, Democratic Republic of Congo in particular, Africa’s medical professionals are experienced in dealing with deadly infectious outbreaks in difficult circumstances, not to mention the continent’s biggest killers – malaria, tuberculosis and HIV/AIDS.
Africa’s public healthcare systems were under immense pressure well before the coronavirus appeared. UN and World Health Organization figures published in 2015, revealed that while Africa had 16% of the global population, it bore 23% of the world’s disease burden, but accounted for only 1% of total global health expenditure.
In April 2001, African governments committed themselves to the Abuja Declaration, undertaking to spend at least 15% of their annual budgets to improve the health sector in their countries. Almost two decades later, and despite some real improvements in the availability and access to healthcare across the continent (Rwanda, Botswana and Zambia had achieved 15% by 2013), Africa’s people have every right to feel short-changed because their governments have largely failed to honour the Abuja Declaration. Even worse, a WHO 2016 report found that 19 countries (including the three countries already mentioned) were spending less than they had before the 2000s. More recently, for example, Nigeria, with impeccable timing, reduced its health budget from 8% to 6% in June this year during the pandemic, citing reduced oil revenues as the reason for the cut.
Still, most African governments were quick to rise to the challenge of halting the spread of COVID-19. But while some countries have clearly succeeded in containing the virus, at least for the time being, with some of the strictest lockdown measures in the world (South Africa and Kenya, for example), others have responded with outright denial (Tanzania) or claims of divine intervention (Burundi). Burundi’s late president, Pierre Nkurunzisa, claimed that God had told him Burundians would not get COVID-19 shortly before he died on 8 June, allegedly due to the virus.
Tanzania’s President, John Magufuli, has taken the novel approach of making the virus go away by the government’s refusal to release any COVID-19 data since May, leaving both the public and scientists in the dark and life to go back to “normal”. In Malawi, meanwhile, an unintended consequence of the country’s lockdown, that included closing schools indefinitely in late March, has been a surge in teenage pregnancies and early marriages.
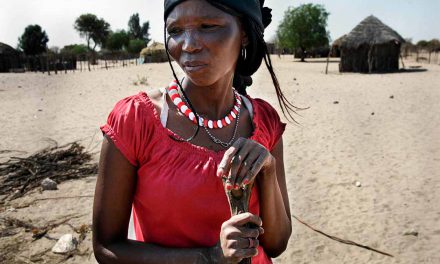
As the UN’s Sustainable Development Goals (SDGs) recognise, poverty and poor health are inextricably linked. According to WHO data, lower respiratory tract infections are among the leading causes of death in Africa, due in part to indoor pollution from cooking using kerosene, biomass or coal when other energy sources are inaccessible or unaffordable. Poverty also makes giving birth a deadly exercise for many women in sub-Saharan Africa who, as contributor Adie Vanessa Offiong writes in ‘Dying to give birth’, account for two thirds of the 87% of the world’s maternal mortalities occurring in Africa and southern Asia. Most of these deaths could be avoided with proper emergency medical intervention.
The advent of COVID-19 has meant that limited and overstretched health resources have been diverted to deal with the pandemic. The WHO estimates that service cancellations due to the virus will lead to a 100% increase in malarial deaths in sub-Saharan Africa and there will be a spike in illness and death from communicable diseases overall.
Complicating matters going forward, a 2019 report in The Lancet reveals that there has been a surge in non-communicable “lifestyle” diseases (NCDs) in Africa over the past two decades, “driven by an increasing incidence of cardiovascular risk factors such as unhealthy diets, reduced physical activity, hypertension, obesity, diabetes, dyslipidaemia and air pollution”. NCDs, The Lancet said, are “set to overtake communicable, maternal, neonatal, and nutritional (CMNN) diseases combined as the leading cause of mortality in sub-Saharan Africa by 2030”.
Diabetes has been found to be a particularly deadly co-morbidity for the virus. For example, in South Africa’s Western Cape Province, 42% of people hospitalised with COVID-19 who also had diabetes had died by mid-July. The International Diabetes Federation says as many as 60% of African adults living with the disease are unaware they have it. In South Africa, for example, the incidence of diabetes rose by 137% between 2017 and 2019.
The figures are alarming, but both the WHO and international health experts insist that despite the devastating consequences of COVID-19, the pandemic could prove to be a positive event in the long run, offering Africa and the rest of the world an opportunity to radically transform their health systems for the public good.
In a timely example of progress, the WHO announced on 25 August that Africa was free of wild poliovirus, eradicating the disease after a long programme of vaccination and surveillance, and with no cases recorded since 2016.
This was good news, but the transformation of health systems post COVID will require political will, knowledge sharing, strong leadership and prioritisation – all of which are too often in short supply in sub-Saharan Africa. Ultimately, one sure sign that Africa’s citizens have the public healthcare they deserve will be when their leaders and members of the elite use their own medical facilities instead of flying off to Hong Kong, Singapore, Switzerland or Moscow for treatment.
Susan Russell is the editor of Good Governance Africa’s quarterly journal, Africa in Fact. She has worked in the media industry for more than 30 years as a journalist, editor, publisher, and as a general manager. Career highlights include several years working for Business Day and more than a decade as a reporter, editor and General Manager at the Sunday Times in Johannesburg.